Telemedicine Pros and Cons
Editor’s note: Alena shows how telemedicine technology is of advantage to healthcare organizations and patients and explains why it is worth investing in. And if you’d like to reap telemedicine benefits, feel free to check out our telemedicine application development offering.
Statistics show the stable growth of the telemedicine market influenced by such factors as the growing demand for online services, the healthcare technological progress, the COVID-19 pandemic, etc. But what exactly makes telemedicine more and more popular: hype or objective benefits? In this article, I will give an overview of the most significant advantages of telemedicine technology, show how telehealth benefits care providers and patients for you to decide whether this technology is worth opting for.
Breaking down telemedicine types
Telemedicine enables remote health care delivery with the help of telecommunications technology. The National Telehealth Resource Center defines the following telemedicine types:
Live Videoconferencing (Synchronous) – two-way interaction between a patient and a healthcare provider using audiovisual telecommunications technology. To see how this type of telemedicine works in real life, check ScienceSoft’s telehealth project for Chiron Health platform.
Store-and-Forward (Asynchronous) – transmission of a patient’s medical information through an electronic communications system to a care provider without a real-time interaction.
Remote Patient Monitoring (RPM) – personal health and medical data collection from an individual outside a medical facility via electronic communication technologies. The collected data is transmitted to a healthcare provider (hospitals, clinics, living facilities, etc.) for use in care and related support. A demo of a telemedicine app with RPM will help you get a better understanding of its functionality.
Pros and cons of telemedicine – let’s look closer
Telemedicine
In-person visits
Pros
– Convenience and accessibility for remote, elderly, or disabled patients
– Real-time monitoring and dynamic treatment planning
– Higher engagement
– Physical exams and hands-on diagnostics
– No location-based barriers, clearer insurance policies
– Better rapport from face-to-face interaction
Cons
– Internet access barriers
– Diagnostic limitations without physical exams
– Regulatory challenges
– Security risks if not HIPAA-compliant
– Less convenient due to the required physical presence
– Less accessible for underserved patients
– Less flexible scheduling
Costs
Often cheaper due to fewer overhead fees
Typically higher per visit, but may include full diagnostics in one appointment, without the need for follow-ups
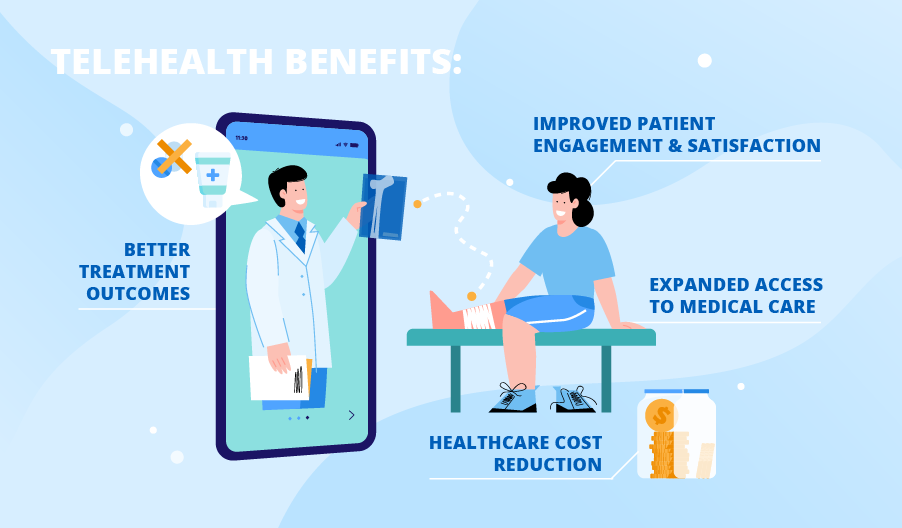
Expanded access to medical care
Since telemedicine is inextricably linked with the use of telecommunications technologies, many barriers to receiving medical care are removed by telehealth technology. For example, telemedicine allows receiving the necessary healthcare services without visiting healthcare providers, which is extremely important for the elderly, people with disabilities, patients from rural areas, post-surgical patients, etc. Patients can use a telemedicine app not only for ordinary e-visits but also for real-time body condition monitoring with the help of wireless medical devices and wearable biosensors. A recent study showed that telehealth significantly improved accessibility to healthcare services, with geographic barriers reduced from 65% to 10%.
Better treatment outcomes
Healthcare providers can achieve an improved quality of care delivery as telemedicine technology allows real-time patient health data monitoring (this online demo shows how it looks in real life). This data can be collected automatically with the help of medical devices or wearable biosensors. Also, personal health data can be added to the system by patients manually. Using relevant information about patients’ physiological parameters, physicians can quickly change or supplement a treatment plan and prescribe necessary medications if needed. In such a way, telemedicine applications can help reduce the readmission rate and emergency room utilization. For example, one study found that symptom severity decreased by 28.6%, and disease-specific markers improved by 8.3% with the use of telemedicine and remote monitoring. In pediatric care, telehealth also helped avoid hospitalizations in 69% of cases and reduced ED visits by 44%.
Healthcare cost reduction
As telehealth reduces emergency room utilization and readmission rate, it helps care providers save quite a lot of money as well. A recent study demonstrated significant cost savings thanks to telehealth and RPM, with direct healthcare costs reduced by 52% (from $25,000 to $12,000) and indirect costs decreased by up to 50% (from under $10,000 to under $5,000). Also, telehealth technology enables care providers to use outsourcing remote analysis services (for example, telepathology and teleradiology) and avoid the cost of specific medical equipment and highly specialized medical staff.
Improved patient engagement and satisfaction
ScienceSoft’s customers note that telehealth solutions make patients feel more secure and confident, as they can reach a care provider with a few clicks and know that their health data is monitored by professionals. Moreover, high-quality telemedicine applications allow patients to participate in their treatment process: patients have access to their treatment plan, information about their vitals with their physician’s comments or suggestions, and relevant educational materials. The positive influence of telehealth technology on the level of patient satisfaction is confirmed by a recent study, where it rose from 80% to 95%.
Lack of internet access
Limited access to reliable broadband remains a significant barrier to equitable telemedicine adoption. As of early 2024, approximately 3% of broadband-eligible locations in the U.S. lack any internet service offering the minimum speeds of 25 Mbps download and 3 Mbps upload required for stable telehealth video visits. Additionally, 6% of fixed internet connections fall below these thresholds, often relying on legacy infrastructure. These limitations are especially common for rural areas, where fewer internet service options and lower-quality connections restrict patients’ ability to participate in virtual care.
Data security concerns
Handling patient data remotely inevitably raises concerns around privacy and security. Unauthorized access, breaches, and insecure communication channels can pose serious threats to the confidentiality of protected health information (PHI). However, these risks aren’t inherent to the technology itself. Just like with any other medical software, security issues typically stem from non-compliance with established privacy standards. When telehealth solutions are developed and used in accordance with HIPAA guidelines, patient information remains protected.
Diagnostic limitations
The lack of a physical exam can reduce diagnostic accuracy in certain situations. While certain cases, such as follow-ups, chronic disease check-ups, or mental health consultations, are well-suited for virtual care, others still require an in-person visit. Some conditions simply can’t be accurately assessed through a screen. For instance, when diagnosis depends on physical examination (checking reflexes, feeling for lumps, etc.), a virtual visit may fall short. In these scenarios, a hybrid care model can serve as a practical solution, blending the convenience of telemedicine with the thoroughness of face-to-face consultations.
Patchwork of state regulations
Finally, regulatory inconsistencies across states add a layer of complexity. For example, payment parity laws, which require insurers to reimburse telehealth visits at the same rate as in-person care, are not standardized nationwide. As of January 2025, only 58% of states have enacted such legislation. This can make access difficult or financially unviable for patients. The story of Maki Inada, a biology professor in New York, highlights the challenge: her Boston-based cancer care team required her to physically be in Massachusetts to legally conduct a telemedicine visit. She was told to drive over five hours to park near the border and take the call from her car. Until reimbursement policies evolve further, these regulatory boundaries will continue to complicate care continuity across state lines.
Leverage telehealth benefits in your app!
As my practice shows, telemedicine applications can be extremely useful for both patients and care providers. Therefore, investing in telehealth software, software product companies have the possibility to enter the healthcare IT market with a profitable product. And to increase the chances for market success, I recommend cooperating with professionals experienced in the development of telemedicine applications. If you are interested, you’re welcome to turn to ScienceSoft’s healthcare IT team to develop your high-quality telemedicine application.
Telemedicine App Development
With decades-long experience, ScienceSoft’s healthcare IT experts are here to design and develop a high-quality telehealth app with advanced features.


